The wait for an organ transplant can be heartbreaking, a race against time that too often ends in heartbreak. But imagine a future where no one must wait, where organs can be built in a lab, tailored for each patient. This once-distant dream is becoming a reality, thanks to groundbreaking advancements in artificial organ development.
In recent years, the fusion of tissue engineering, biotechnology, and regenerative medicine has turned science fiction into science fact. These innovations are reshaping the healthcare landscape, offering hope to millions who need a second chance at life. They could end the global organ shortage crisis and promise revolutionary treatments for diseases and a better quality of life for countless people.
The journey of artificial organ creation is more than just a scientific breakthrough, it’s a testament to human ingenuity and our relentless drive to solve life’s most complex problems. From 3D-printed hearts to lab-grown kidneys, every step forward carries the potential to transform despair into hope and waiting into healing.

The Need for Artificial Organs
Every year, thousands of people around the world die while waiting for an organ transplant. According to the World Health Organization (WHO), approximately 130,000 organ transplants are performed annually, yet millions remain on waiting lists. The gap between organ donors and patients needing transplants is widening, driving scientists to search for alternative solutions. Artificial organs, specifically those that can be bioengineered to function like human organs, offer a potential solution to this crisis.
Developments in Artificial Organ Technology
Bioengineering and 3D Printing
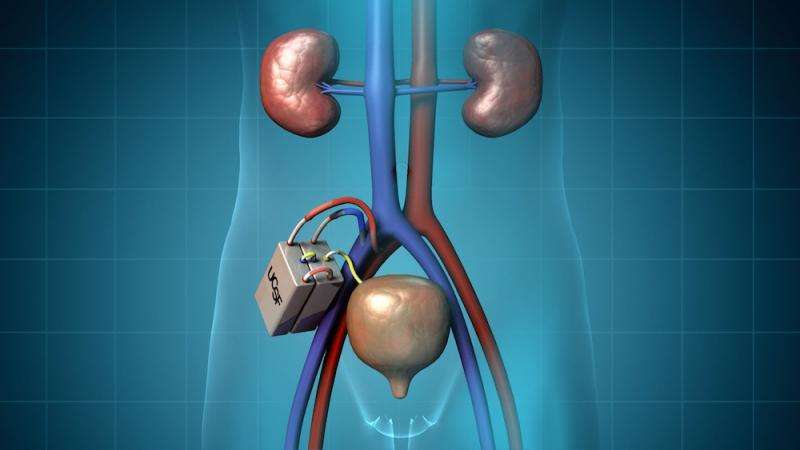
One of the most promising advancements in artificial organ development is bioengineering and 3D printing. Scientists have made significant strides in creating tissues and organs by combining cells with synthetic materials. The idea is to print or grow cells in a scaffold, which develops into a functioning organ.
This method allows the manufacturing of complex tissues such as the heart, liver, and kidney. 3D bioprinting has been used in constructing these organs layer by layer, providing precise control over their structure and function. In 2019, researchers successfully printed a human heart prototype using 3D printing technology, demonstrating that organs could be fabricated with similar complexity as natural tissues.
Organ-on-a-Chip Technology
Another breakthrough is the development of organ-on-a-chip technology. These miniature devices replicate the structure and function of human organs on a small, lab-grown platform. Using living cells, these chips mimic how an organ works, making them invaluable for testing drugs, understanding diseases, and even creating potential artificial organs.
Researchers are now working to integrate several organ models into one system to simulate the complex interactions between different body systems, offering hope for creating composite organs for transplantation.
Stem Cell Research and Regenerative Medicine
Stem cell research has been central to the development of artificial organs. Stem cells have the potential to differentiate into various types of tissues and organs. By harnessing the power of stem cells, scientists are investigating ways to grow human tissues and even whole organs in the lab.
For instance, artificial kidneys are being developed by using stem cells to generate nephrons, (the functional units of the kidneys). In 2023, they develop kidney-like structures in a laboratory, paving the way for future kidney regeneration.
In parallel, regenerative medicine focuses on enhancing the ability of the body to repair or replace damaged organs by stimulating natural healing processes. This includes the development of biocompatible scaffolds that guide tissue regeneration and gene editing techniques like CRISPR to promote tissue growth.
Challenges and Ethical Considerations
Despite incredible progress, developing artificial organs that can fully replicate human ones remains a daunting challenge. Scientists have successfully created tissues and small prototypes, but replicating the complexity of organs like the heart or liver is far more difficult.
One of the biggest hurdles is constructing a network of blood vessels, known as vascularization that can keep these organs alive and functioning. Without an efficient blood supply, even the most advanced artificial organs cannot survive long-term or perform as needed.
Beyond the technical obstacles, ethical and regulatory concerns add layers of complexity. Questions arise about using human cells, modifying genetics, and relying on animals like pigs to grow organs. These innovations spark debates about animal welfare, genetic tampering, and the unknown long-term effects of such procedures.
On top of that, regulatory agencies like the FDA require rigorous testing, but the speed of innovation often outpaces existing rules, leaving gaps in oversight (U.S. Department of Health and Human Services, 2022). Overcoming these challenges is essential to make artificial organs a safe, accessible, and transformative option for those in need.
The future of healing is being built, organ by organ
The Future of Artificial Organs
Artificial organs are transforming medicine, with promising developments on the horizon. Personalized medicine could allow organs to be crafted from a patient’s cells, reducing rejection and improving transplant success. Fully synthetic organs made from bioengineered materials may one day replace the need for donors, offering greater durability and reliability.
Additionally, integrating artificial organs with robotics and AI could create advanced systems that monitor and adjust organ function in real-time, optimizing patient outcomes and improving quality of life.
Conclusion
The development of artificial organs is revolutionizing medicine, bringing us closer to a future where organ shortages are a thing of the past. Imagine a world where failing hearts or kidneys are replaced with lab-grown organs tailored to each patient. While challenges remain, each breakthrough offers new hope, turning what once seemed impossible into a life-saving reality.
References:
- Kim, D. H., Ahn, J., Kang, H. K., Kim, M. S., Kim, N. G., Kook, M. G., Choi, S. W., Jeon, N. L., Woo, H. M., & Kang, K. S. (2021). Development of highly functional bioengineered human liver with perfusable vasculature. Biomaterials, 265, 120417.
- Soto Veliz, K. Lin, C. Sahlgren, Smart Med. 2023, 2(1),e20220030. https://doi.org/10.1002/SMMD.20220030
- https://www.weforum.org/stories/2019/04/researchers-create-first-ever-3d-printed-heart-using-human-tissue/
- https://doi.org/10.1016/j.stem.2019.05.016. (https://www.sciencedirect.com/science/article/pii/S1934590919302206)
- de Kanter, A. J., Jongsma, K. R., Verhaar, M. C., & Bredenoord, A. L. (2023). The Ethical Implications of Tissue Engineering for Regenerative Purposes: A Systematic Review. Tissue engineering. Part B, Reviews, 29(2), 167–187. https://doi.org/10.1089/ten.TEB.2022.0033
- https://data.hrsa.gov/topics/health-systems/organ-donation
- Tripathi, S., Mandal, S. S., Bauri, S., & Maiti, P. (2022). 3D bioprinting and its innovative approach for biomedical applications. MedComm, 4(1), e194. https://doi.org/10.1002/mco2.194
More from the Author: Organizing Patient Data Management and AI-driven Diagnostics

Sadaf Sarfraz, currently a lecturer, holds an MPhil in Molecular Pathology and Genomics, complemented by a BSc in Medical Laboratory Technology. Contributing as a healthcare writer at Scientia-Pakistan, she passionately engages in calligraphy and art.

