It was a sunny July afternoon when Sameer, a 45-year-old resident of Swat, rushed his mother to a nearby private hospital because her chest pain was becoming unbearable. However, the hospital quoted treatment costs that were two-thirds of Sameer’s monthly income. Overwhelmed by his mother’s falling health, he took his mother to a public hospital, where the area was already overcrowded.
He stood in line with his head bowed down, grappling with unspeakable feelings as he waited for his turn to obtain an emergency slip. After a few moments, he was handed a list of necessary investigations and medications, which were far beyond his salary and savings. At that moment, his emotions peaked; the weight of unsaid words hung on his tongue as he whispered with a heavy heart, “How can I pay for my mother’s life, provide food for my children, or endure the unending pain of debt?”
This moment captures a glimpse of the millions of people like Sameer who face similar situations daily. They sell their jewelry, livestock, and gamble with their savings to cover medical expenses. Although we advocate for “health for all,” the reality remains a harsh struggle between paying for life and falling into poverty. Stories like these raise alarm bells for Universal Health Coverage every day.
What is Universal Health Coverage?
Universal health coverage means that everyone has access to essential health services without facing financial hardship. The World Health Organization defines it through two main domains: service coverage and financial protection. It is not a luxury or a charity; it is a basic human right. Universal health coverage ensures that families can access essential healthcare without risking a financial downturn that leads to poverty.
Why is it so Important?
Imagine walking on a tightrope with a safety net beneath you to catch you if you fall. The tighter and broader the safety net, the greater the chances it will prevent you from experiencing a traumatic fall. Health emergencies—such as heart attacks, stroke, complications during childbirth, and chronic diseases like kidney failure, thalassemia, and cancer—can deplete your savings and possessions, potentially driving you into poverty.
Universal health coverage acts as a safety net, minimizing your financial burdens during these crises. It transforms health care from a gamble into a guarantee, ensuring that health shocks do not trap you in lifelong poverty.
How it Affects Our Health System and Economic Growth
Universal Health Coverage (UHC) is a basic human right that is so crucial that the World Health Organization (WHO) has included it in its Sustainable Development Goals for 2030. Efficient health coverage ensures a healthy population, which leads to greater productivity, economic growth, and a reduction in early school dropouts, child labor, and other social issues. However, gaps in UHC have dire consequences, resulting in a shortage of healthcare staff, medicines, and decaying infrastructure.
This situation forces patients to incur out-of-pocket expenses, trapping them in a cycle of debt and poverty for many years. This leads to delays in seeking care, causing serious diseases to go undiagnosed until they reach a fatal stage. Even when diseases are diagnosed at advanced stages, the immense financial burden of treatment places an unbearable strain on low-income families, turning a diagnosis into a death sentence.
Populations with inadequate Universal Health Coverage (UHC) experience delays in immunizations and insufficient healthcare, leading to higher rates of mortality and disabilities. According to the World Health Organization (WHO), during the COVID-19 pandemic, weak health systems resulted in 25 million children missing routine vaccinations in 2021.
By mid-2023, only 34% of individuals in low-income countries had received COVID-19 vaccinations, compared to 73% in high-income countries. Additionally, countries with high out-of-pocket healthcare costs saw approximately 344 million people fall into extreme poverty and 1.3 billion people into relative poverty in 2019 due to medical expenses.
Therefore, the WHO and its partners emphasize that health spending should be viewed as an investment rather than a cost and must be prioritized.
What’s Happening in Pakistan?
Universal health coverage is a pressing issue in war-affected countries like Pakistan, where funding for this purpose is limited. Unfortunately, public hospitals in Pakistan are severely underfunded, with the country spending less than 1% of its GDP on public health.
This is in stark contrast to the World Health Organization’s recommendation of spending 5% of GDP on basic and universal health coverage. As a result, financial coverage for healthcare is inadequate, leading to an overwhelming dominance of private hospitals in healthcare expenditures.
Pakistan’s health sector has approximately 52.6% of health expenditure that is private, and nearly 89% of it comes directly out of patients’ pockets. This situation forces families into a cycle of illness, debt, and poverty.
What are real-life stories?
Chronic underfunding leads to multiple gaps in the safety net of Universal Health Coverage, causing families to fall into poverty due to healthcare-related expenses. For instance, Kashif explains that his three-year-old son suffers from recurrent chest infections due to a genetic disease. Each time he is admitted to the hospital, the treatment costs him around two-thirds of his monthly income.
Sometimes, government hospitals are so overcrowded that there are no available beds, even for sharing with other patients. As a result, he has to admit his son to a private hospital, further worsening his financial situation and leaving him in debt that he has yet to pay off.
Dr. Zia Ullah, a resident pediatrician, states that these soaring expenses at government hospitals deter families from seeking treatment, leading them to rely on unqualified practitioners, which further exacerbates their children’s conditions.
The financial burden from these healthcare costs often drives parents into poverty, forcing them to rely on less nutritious food for their children, resulting in malnourished kids. This creates a cycle that can lead to a future generation plagued with various diseases and ultimately a less productive society.
Similarly, Niaz Ali, a rickshaw driver, shares that he suffers from diabetes and needs five to eight insulin shots each month, which cost him one-third of his income. This financial burden forces him to rely on charity for his treatment. At times, he has to skip doses because he has to choose between buying medicine and paying for his children’s school fees, putting himself at risk of severe consequences.
The situation becomes even worse for expectant mothers who need proper nutrition and healthcare. Razia, a 33-year-old mother, says it costs them around 8,000 rupees just to travel to the hospital for antenatal care. The additional costs for ultrasounds, investigations, and other medications exhaust their savings from daily wages, leading them to rely on less nutritious food and sometimes skip meals. This results in serious consequences, jeopardizing both the mother’s and the child’s health.
“Many families defer prenatal care, which can often lead to stillbirths, miscarriages, and genetic diseases that could be prevented with early interventions”, says Dr Iqra, who is a resident gynecologist.
These aren’t isolated tales; they reflect the everyday reality for millions of people. When illness strikes, many households are forced to sell livestock or land, cut back on food, or abandon education to pay for medical expenses. Poorer families suffer the most, as treatment and medication are often unaffordable without support. This vicious cycle of illness → debt → poverty—will persist unless public funding is significantly increased.
What are Pakistan’s Initiatives?
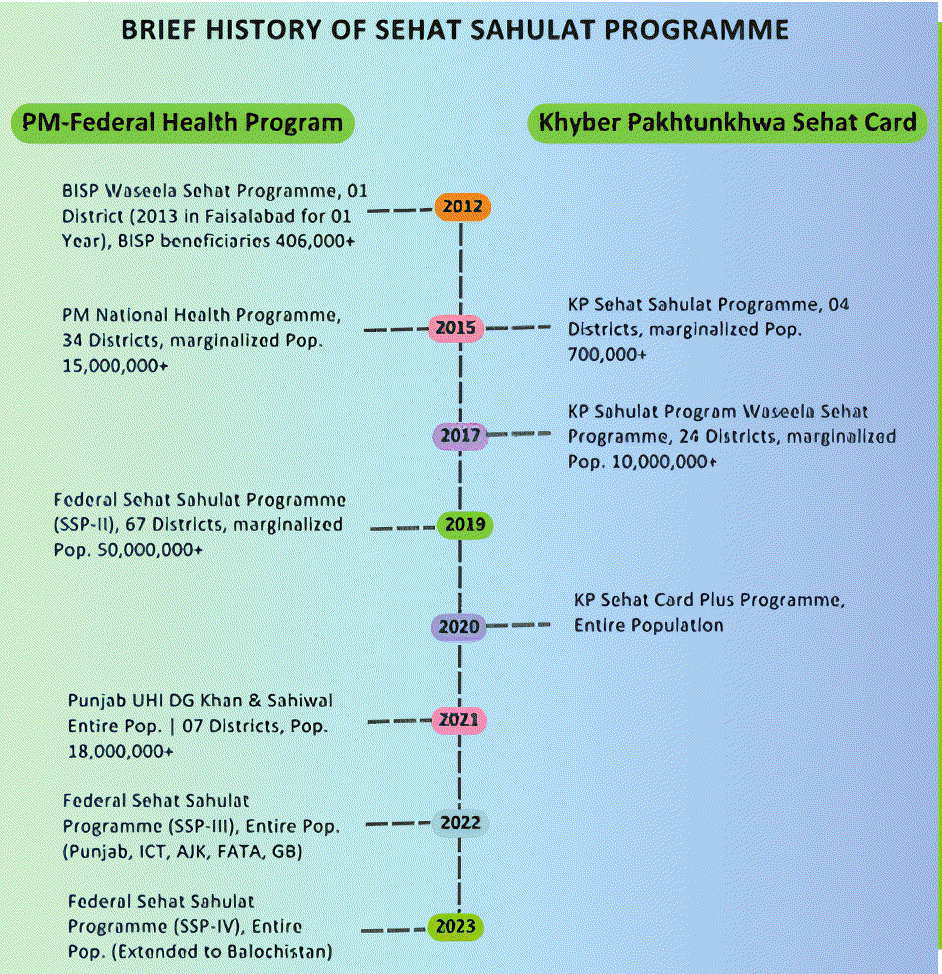
In response to various healthcare crises, Pakistan has launched multiple initiatives. In 2015, the Khyber Pakhtunkhwa (KPK) government launched the Sehat Sahulat Programme (SSP) to cover healthcare expenses for individuals from targeted groups. This initiative later expanded to other provinces in Pakistan. In 2020, it was made universal for all residents of KP, and later, the federal government also expanded it to the entire population in 2022.
The inclusion of private hospitals in this program has made it more appealing, as these facilities often have better infrastructure and equipment and are more accessible than government hospitals. This has enabled people to access private healthcare services, similar to those available to higher socioeconomic groups.
Moreover, the recent increase in funding for this program in the KP government budget, from 28 billion to 35 billion, along with an extra 6 billion for the merged districts, marks a significant step toward ensuring its sustainability. As a result, healthcare has become more accessible, and many people are now seeking medical services through this program.
For instance, Abdul Wahab mentioned that he underwent three surgeries under the Sehat Card Plus Programme, which cost him very little compared to a previous surgery that had taken up two months’ worth of his salary. The inclusion of C-sections, normal deliveries, post-operative care, and other maternal surgeries has made these services more appealing, as more mothers are opting for them. This choice helps prevent delivery complications and reduces maternal mortality, thus improving maternal and child healthcare.
Similarly, surgeries such as appendectomies, gallbladder removals, and tonsillectomies, which were previously performed infrequently, have seen a significant increase in demand. More people are choosing these procedures under the Sehat Card, allowing them timely intervention and preventing potential complications.
Furthermore, the inclusion of transplant operations—such as liver, kidney, bone marrow, and cochlear implants—has made this initiative groundbreaking, as these surgeries are essential for improving the quality of life for patients who depend on them.
A recent 2024 report on Universal Health Coverage (UHC) in Pakistan indicates that the Service Coverage Index stood at 53.9 by the end of 2023, reflecting a 35.8% improvement since 2015 and a 2.2% increase since 2022. Although we are progressing at a relatively slow pace, this progress warrants recognition. Advancing towards UHC is a continuous effort, and acknowledging these improvements is more significant than simply achieving the goal itself.
What are the pitfalls of these initiatives?
Although these insurance initiatives have yielded promising results, the program still encounters a few challenges. Dr Seema Mohmand, a public health expert, notes that most of the participating hospitals in these programs are private. This situation means that the government is funding the private sector more than it is supporting public hospitals.
The funds for these initiatives come from the total health expenditure, leading to a focus on insurance activities rather than improvements in primary healthcare facilities. She stated that government funding is equally distributed among both the poor and the rich, which is depleting many resources. With this approach, universal health insurance may become unsustainable amid rising inflation.
Additionally, Dr. Mohmand explains that there is a lack of monitoring and accountability for these initiatives, which can result in the overuse of costly procedures performed under the program. Without proper oversight and accountability, these initiatives may struggle to break the cycle of poverty. She emphasizes that our primary aim should be “to strengthen our healthcare facilities so that even the poorest individuals can access services without having to choose between health and poverty.”
Voices from the Field
Although progress has been made in achieving Universal Health Coverage (UHC), out-of-pocket health expenditures still account for 48.86% of total health spending. Dr. Seema Mohmand emphasizes that while UHC initiatives typically target large hospitals, there should be a particular focus on primary health care, which is a fundamental pillar of UHC. The poor in rural areas rely on these free clinics, and strengthening them would help us achieve significant breakthroughs in UHC.
Dr Awais, a public health expert, points out that healthcare funding issues from less than 1% of our GDP. With such limited funding, we cannot expand our insurance schemes to achieve UHC; substantial new budget support is essential. The government should make concerted efforts to upgrade hospital infrastructure, improve the affordability and availability of emergency medicine, and ensure access to imaging machines, electricity, and adequate staff.
These improvements are crucial so that people do not have to wait in emergency or outpatient departments while their loved ones struggle for life. Strengthening our hospitals is vital for achieving our UHC goals.
Charting the Way Forward: What Strategies Should We Adopt?
According to Dr Seema Mohmand, to break the vicious cycle of illness and poverty, policymakers must allocate more than 1% of GDP to healthcare. Health is a basic right for every individual, regardless of their financial situation. Policymakers should work to increase health funding to meet the 5% GDP goal recommended by the WHO. Special emphasis should be placed on diverting funds to primary healthcare and public hospitals so that the rural population can benefit as well.
She outlined the following key strategies:
- Investment in Primary Healthcare: Strengthening local clinics, implementing preventive strategies, and training community health workers can yield significant health improvements at a low cost. This approach would greatly reduce out-of-pocket expenses, making the “Health for All” initiative a reality.
- Increase Health Budget: Raise the health budget above 1% of GDP and view this as an investment that can produce broader economic benefits. Consistent efforts should be made to gradually increase health budgets without applying cuts. Tax revenues from tobacco and sugary drinks could be redirected to fund the health sector.
- Expand Health Insurance: Extend health insurance programs to rural areas and local clinics to prevent diseases and minimize the transportation costs for patients traveling to larger hospitals. Ensure that the Sehat Sahulat programs are funded consistently and remain unaffected by political instability.
- Limit the services to low-income individuals. Given the country’s significant debt and the large portion of our budget directed towards interest payments, it will be challenging to sustain universal health insurance if we provide equal services to all citizens. Therefore, policymakers should focus on serving the underserved, poor, and marginalized populations to alleviate the financial burden and ensure continuous funding for this program.
- Promote competition among insurance companies. Currently, State Life Insurance Corporation (SLIC) is the only provider responsible for these services, raising concerns about its performance. Relying on a single company hinders the potential for innovative solutions. The government should encourage the involvement of multiple insurance providers to foster fair competition and enhance the quality of services offered.
- Develop a national health financing network. There is currently no consensus regarding the future of this program, which is often influenced by political dynamics. A comprehensive roadmap should be established, incorporating input from all provinces and major stakeholders, to create a plan that minimizes political interference and ensures the program’s continuity, regardless of changes in government.
- Invest in Public Infrastructure: Improving public healthcare facilities by enhancing staffing, providing adequate medical supplies and equipment, and ensuring bed availability so that the poorest individuals can receive treatment without having to revert to private healthcare.
- Establish New Healthcare Facilities: The government should work to establish new healthcare facilities, aiming to provide services through public-private partnerships.
- Support Local Pharmaceutical Companies: Assist local pharmaceutical and biotech companies to ensure affordable pricing for life-saving medications. Price control should be regulated and prevent shortages of essential medicines.
- Leverage Technology: With the evolving landscape of healthcare, artificial intelligence and telemedicine should be integrated effectively. Clinicians and developers must collaborate to advance health technologies.
- Strengthen International Collaboration: The government should enhance partnerships with international agencies such as the WHO and UN to secure aid and support for expanding universal health coverage. Agreements should be made with companies, facilitated by these organizations, to ensure access to innovative treatments, vaccines, and cutting-edge technologies at an affordable cost.
Call to Action
To the policymakers: Your decisions are crucial. Expanding healthcare funding can mean the difference between millions of families, like Sameer’s, facing bankruptcy or walking out of hospitals with hope. Your actions today can shape the future for generations to come.
To the pharmaceutical and technology companies: Your products must combine hope with affordability. Creating innovative breakthroughs without ensuring affordability is merely a business strategy, not a commitment to safeguarding lives.
To the service providers and the general public: The government is making significant efforts to ensure access to healthcare and minimize the financial burden on citizens. Your cooperation is crucial for the successful delivery of these services. It is essential to prevent fraudulent insurance claims and reduce the irrational use of services solely for insurance benefits. The general public is encouraged to use these healthcare privileges responsibly and only when necessary.
To the science writers: Your stories play a vital role in highlighting these gaps and holding policymakers accountable. Your voice matters and can influence the future.
Universal health coverage is a basic human right and a smart investment, yet it remains elusive in war-affected, low socioeconomic countries like Pakistan. The stories of individuals like Sameer highlight the urgent need for its implementation. Although some progress has been made, without proper financing, accountability, and improved health budgets, these initiatives will only provide superficial hope amid a growing population.
By reinforcing primary care, expanding insurance coverage, and ensuring access to treatments for the most vulnerable, we can turn the “health for all” slogan into a reality. The 2030 Sustainable Development Goals demand bold changes in our healthcare policies. Let’s take action now, so no Pakistani family ever has to choose between medicine and meals.
References:
- https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc)
- https://www.finance.gov.pk/survey_2025.html
- https://www.pbs.gov.pk/content/national-health-accounts
- https://sehatsahulat.com.pk/sehat-sahulat-programme-history/
- https://www.pakp.gov.pk/wp-content/uploads/2025/06/cb-White-Paper-2025-26.pdf
- https://www.nhsrc.gov.pk/SiteImage/Misc/files/2_%20Brief_Trend_Analysis.pdf
- https://www.dawn.com/news/1884211
More from this Author: Swat Flood Tragedy: A Wake-Up Call on Climate Change, not a Headline to Forget

Yasir Ahmad is a final-year MBBS student with a strong passion for science writing. He is dedicated to finding innovative ways to communicate complex topics, including climate issues and health. He was a former science writing intern at Scientia Cohort 4. His goal is to make important scientific information accessible in a clear and engaging manner.

