People often confuse the brain with the ‘mind’. And it is, for a fact, used interchangeably. Science literature obviously recognizes nature and what constitutes the ‘mind,’ but the impact is still not enough to be cemented into the subconscious of science-acclimatized people, let alone the lay folk. The brain is generally called the mind since it contains the immense and almost limitless intricate network of neurons that perceive, process, and execute decisions.
However, we have overlooked (for the mainstream at least) the presence of a complicated neural network within the gut wall. How this network works in synchrony with the workings of the brain and how it is affected by different influences will be discussed here. One of the influences is the presence of gut microbiota (bacteria, archaea, viruses, and fungi).
To understand this influential relationship, we must understand the hows and whys of the nervous system and Microbiota. We will find out why sayings like ‘you are what you eat’ and ‘butterflies in the stomach’ do make practical and scientific sense.
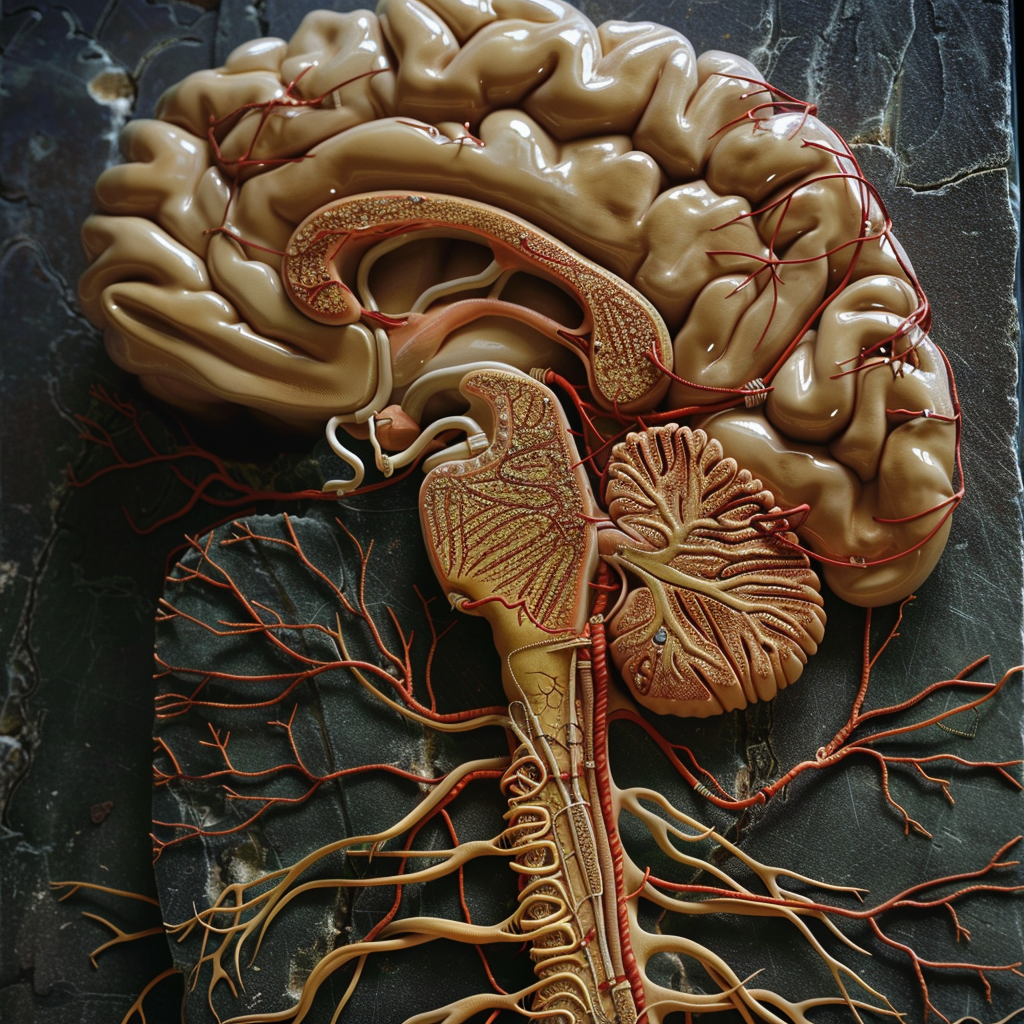
The nervous system
The nervous system in the human body consists of central and peripheral constituents. The central part is comprised of the brain and the spinal cord. The peripheral part consists of the autonomic (ANS)(network of nerves that regulates involuntary activities in the body) and peripheral nervous system (PNS). The peripheral nervous system consists of the numerous nerves that serve the voluntary functions of muscles and arise from the brain and spinal cord.
The enteric nervous system (ENS) present in the gut wall from the esophagus to the anus is part of the ANS. This is an extensive meshwork of neurons embedded within the gut, approximated to be 200-600 million in number, having a bidirectional relationship with the brain (sometimes referred to as the second brain)1. Along with regulating the inherent processes of the gut, like digestion and absorption2, these neurons influence the brain’s neurochemistry.
Meanwhile, the brain regulates these neurons through this feedback loop3. This axis has been referred to as the Gut-Brain axis (GBA). However, the ‘Mind’ referred to hitherto in the article also refers to this complex whole of the brain and the enteric nervous system, emphasizing this astonishing fact that how we behave, think, and act is not only orchestrated by the brain but also by what is in our bellies.
The Microbiota (the germs within)
The human body is a ‘super-organism’. It is said to host around 1014 bacterial cells within the gut, which outnumbers the human cells by a factor of 10. The same goes for the bacterial genome in the human gut, which is estimated to be approximately 100 times more abundant in the human body than the human genome itself. The organisms and humans live together in a symbiotic relationship where the gut environment provides shelter to them, and they exercise their numerous crucial roles. Some roles include regulating the immune, metabolic, and enteric nervous systems and the synthesis of vitamins4.
In addition, these microorganisms have a role in maintaining the integrity of the epithelial gut wall. This protection is invaluable in maintaining a barrier between certain ‘bad’ organisms in the gut and the blood. To benefit us, the Microbiota requires a certain balance between the different phyla, out of which Bacteroidetes and Firmicutes make up more than 90 percent of the total load in the guts5.
In addition to the bacteria, numerous fungi are populating the gut: Saccharomyces and Candida, to name a few. These exist in an existential harmony with the bacterial colonies to produce a state of balance within the gut and throughout the body. This state of balance of ‘homeostasis’ we keep referring to hinges on the harmony within the flora of the gut in terms of numbers and function.
Consider the reverse now or ‘dysbiosis,’ where the Microbiota is disturbed, which could happen for a multitude of reasons. One could be the use of antibiotics, which, as we know, act against bacteria, and as previously mentioned, our gut is loaded with them. Then there comes the fact that whatever we eat is also eaten and processed by the flora in our gut, and they are also picky eaters for their well-being. These bacteria process food and nutrients and produce chemicals that maintain a state of balance in the gut and the body. The nervous and immune systems’ well-being depends direly on this.
If we feed them harmful chemicals, the ‘good ones’ die out, and the ‘opportunist’ ones start increasing in number. These ‘opportunists’ render the harmonious environment redundant. Local inflammation starts to creep up, and problems of indigestion and malabsorption appear. In addition to this, the whole regulation of the enteric nervous system is dysregulated by the ‘dysbiosis’6. This will be explored later.
The human body is a ‘super-organism’. It is said to host around 1014 bacterial cells within the gut, which outnumbers the human cells by a factor of 10. The same goes for the bacterial genome in the human gut, which is estimated to be approximately 100 times more abundant in the human body than the human genome itself.
The Bi-directional link between the Brain and the enteric nervous system
The brain has a two-way highway between it and the enteric nervous system. To keep it simple, the brain feels what the gut feels, and the gut feels what the brain feels. The gut wall has a meshwork of neurons and its network, which senses even the subtlest of changes in the environment, and this is signaled to the brain, which in turn sends back signals to the gut for the effector response7. Changes in the gut can include changes in the flora, pH, or quantity/quality of food. This to-and-fro feedback loop is in addition to the local responses the ENS puts up, which include hormone/neurotransmitter secretion trying to adapt to the changing gut environment.
It is fascinating to note that the gut’s internal state profoundly affects the brain’s internal state. For example, the type of food we eat can, as we know, directly influence our moods and neurocognitive parameters through the blood after being absorbed. However, the local environment created in the gut by the foods we eat can also affect the brain state. The effector responses in the brain could be the release of or inhibition of the ‘happy’ or ‘pleasure’ hormones like serotonin and dopamine.
This results in a feedback loop whereby the state of the mind then influences how our gut acts in its functions. A depressed person is more likely to have a disturbed gastrointestinal (GI) than someone who is not. The ‘Mind’ thus is not just that chunk of fat in our skulls; it is a complex whole, with a synchronized control, between the brain and the ENS.
Influence of Microbiota on the ‘Mind’
The gut microbiota and its role in the normal functioning of the ENS and the brain have been studied extensively over the years. The gut, where they are located, has mainly been postulated to be the primary site of pathologies that give rise to neurodegenerative diseases like Alzheimer’s, Parkinson’s disease, and autism. Metabolic diseases like diabetes mellitus and even cancers are also considered to arise because of the inflammation in the gut wall, which occurs due to dysbiosis8. The microbiota release neurotransmitters and products of their metabolism of food, like short-chain fatty acids (butyrate, propionate, and acetate).
These play vital roles in the stability of the gut blood barrier, preventing inflammation and sending positive feedback signals to the brain that ‘ all is well9. Interaction between the bacteria and their products of metabolism occurs via specific receptors, which leads to the regulation of nerve function in the ENS. This is especially relevant when, in the setting of dysbiosis, pathogenic strains of bacteria, which generally are suppressed by the ‘good guy’ bacteria, start producing toxins that trigger inflammation in the gut-blood barrier and, through the ENS, may affect brain function through the feedback loops previously mentioned.
It has been shown in mouse models that microbiota-ENS interaction may facilitate CNS development during early years. This is evidenced by abnormal ENS architecture in mice made ‘germ-free’ mice, in whom reduced neuron density was also noted in studies10. Neuroactive molecules regulate nerve signals and affect neuropsychiatric parameters such as sleep, mood, and cognition. Chemicals (i.e., dopamine, serotonin, etc.) related to mood in different critical areas of the brain are regulated by the Microbiota of the gut7. One example which deserves mention here is the condition called ‘Irritable bowel syndrome (IBS)’.

A condition of increased gut sensitivity to pain, which may or may not be associated with altered bowel habits and function. It has been shown that stress, especially early life stress, can predispose one to this condition. It has been demonstrated in rats that the Hypothalamic-pituitary-adrenal axis, when activated during stress (can be due to cytokines or external factors), releases cortisone, which leads to a change in the Microbiota and release of neurotransmitters in the gut, which alter gut movements.
This, in turn, creates a positive feedback loop whereby more cortisone is produced and more changes in the gut environment. The lack of certain bacteria in the Microbiota has been shown to predispose to depression/anxiety. This mechanism has been observed in depression/anxiety models of rat studies, which highlights the complex processes behind IBS7. Administration of certain bacteria, antidepressants, and cognitive behavioral therapy (CBT )11 can mitigate the exaggerated cortisone response and also, hence, the whole cascade.
Practical implications
It is quite evident that a healthy microbiota profile is essential to maintain the integrity of the ENS and its connections with and influence on the brain. In lieu of the said, maintaining a balanced & healthy lifestyle cannot be overemphasized. This includes living a life where stress is adequately managed, getting good quality sleep, and eating a balanced diet, which includes a generous amount of pre- and pro-biotics. Prebiotics are basically foods that contain high-quality fiber, which serves as food for the ‘good guy’ bacteria in our gut.
It would make sense to increase the number of the density of these by serving them the food they need. Examples include apples, bananas, onions, asparagus, etc. Probiotics, on the other hand, are live microorganisms that, when added to our diet, can naturally increase the number and diversity of microbiota and impart health benefits. Examples include mostly fermented foods (where bacteria and yeast convert carbohydrates into acids or alcohol) such as sour cheese and cream and dark chocolate, etc.
What is important to note is that foods like yogurt that are commercially available may not actually have the bioavailable probiotics mentioned due to the processes of heat treatment, preservatives, and sugar additives. ‘Kefir’ yogurt (a variety made from milk that is fermented longer than the usual yogurt) has three times more probiotics than traditional yogurt, especially more ‘live’ cultures.
Our guts play a central part in the nexus of neural control of our very beings, so next time you go shopping for food, remember, it is not only your gut that you will serve; it is your mind!
References:
- J.B. Furness, B.P. Callaghan, L.R. Rivera, H.J. Cho
- The enteric nervous system and gastrointestinal innervation: integrated local and central control.Adv. Exp. Med. Biol., 817 (2014), pp. 39-71
- Fleming MA 2nd, Ehsan L, Moore SR, Levin DE. The Enteric Nervous System and Its Emerging Role as a Therapeutic Target. Gastroenterol Res Pract. 2020 Sep 8;2020:8024171. doi: 10.1155/2020/8024171. PMID: 32963521; PMCID: PMC7495222
- M.J. Caycho Salazar F, Herrera-Covarrubias D, A. Coria-Ávila G, I. García-Hernández L, Rebeca Toledo-Cárdenas M, Elena Hernández-Aguilar M, et al. The Brain-Like Enteric Nervous System [Internet]. Topics in Autonomic Nervous System. IntechOpen; 2023. Available from: http://dx.doi.org/10.5772/intechopen.112571
- Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J. 2017 May 16;474(11):1823-1836. doi: 10.1042/BCJ20160510. PMID: 28512250; PMCID: PMC5433529.
- Rinninella E, Raoul P, Cintoni M, Franceschi F, Miggiano GAD, Gasbarrini A, Mele MC. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms. 2019 Jan 10;7(1):14. doi: 10.3390/microorganisms7010014. PMID: 30634578; PMCID: PMC6351938.
- Lobionda S, Sittipo P, Kwon HY, Lee YK. The Role of Gut Microbiota in Intestinal Inflammation with Respect to Diet and Extrinsic Stressors. Microorganisms. 2019 Aug 19;7(8):271. doi: 10.3390/microorganisms7080271. PMID: 31430948; PMCID: PMC6722800.
- Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015 Apr-Jun;28(2):203-209. PMID: 25830558; PMCID: PMC4367209.
- Steven Fried, Eve Wemelle, Patrice D. Cani, Claude Knauf, Interactions between the microbiota and enteric nervous system during gut-brain disorders, Neuropharmacology, Volume 197, 2021, 108721, ISSN00283908,https://doi.org/10.1016/j.neuropharm.2021.108721.(https://www.sciencedirect.com/science/article/pii/S0028390821002768)
- Silva Ygor Parladore, Bernardi Andressa, Frozza Rudimar Luiz.The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication.Frontiers in Endocrinology.Volume 11,2020.https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.00025.DOI=10.3389/fendo.2020.00025.ISSN=1664-2392
- Niall P. Hyland, John F. Cryan, Microbe-host interactions: Influence of the gut microbiota on the enteric nervous system, Developmental Biology, Volume 417, Issue 2, 2016, Pages 182-187, ISSN 0012-1606, https://doi.org/10.1016/j.ydbio.2016.06.027.(https://www.sciencedirect.com/science/article/pii/S0012160616301518
- Kinsinger SW. Cognitive-behavioral therapy for patients with irritable bowel syndrome: current insights. Psychol Res Behav Manag. 2017 Jul 19;10:231-237. doi: 10.2147/PRBM.S120817. PMID: 28790872; PMCID: PMC5530860.
Similar Posts: AI and Neurobiology: Understanding the Brain through Computational Models
Dr Syed Hunain Riaz is a Physician with expertise and experience in Endocrinology & Metabolism with a passion for eliciting change through the dissemination and application of precise knowledge. He is a space enthusiast, avid reader, blog writer, amateur photographer ( Astro & every day), and gamer.
Writing interests include preventive & lifestyle medicine and psychosocial issues. Dr. Hunain believes in limitless creativity and productivity of the human mind. Nature of consciousness, reality, and patterns in the universe are areas of special interest. He can be reached at syedhunain@gmail.com