Twenty-seven-year-old Muhammad Usman from Lahore picked up Cutaneous Leishmaniasis (CL) after traveling to Multan where CL is more prevalent. Lesions started appearing on his face. He immediately visited the hospital, where they performed a biopsy of the lesions. The results were negative and his family just neglected these lesions because they were painless. Subsequently, the lesions began manifesting on the other body parts.
After two months some nodules converted into ulcers and got filled with pus. He was admitted to the hospital as the condition was getting worse day by day. They left the hospital and returned home due to the prolonged delay in getting medical attention.
This time he visited another hospital and had his biopsy at a private lab. He was declared positive for CL. The doctor advised him to try Medecins Sans Frontiers (MSFs) leishmaniasis services in Peshawar. He spent 37 days in Peshawar and during his stay, the staff treated him professionally and his face gradually became spotless. [1]
Usman was stigmatized since the people around him avoided shaking hands with him and he suffered financially as well [1]. A study found that people with CL are judged as dirty, impure, and contagious [2].
What are NTDs?
Neglected tropical diseases (NTDs) are a group of 20 conditions caused by many pathogens including bacteria, viruses, fungi, protozoa, and toxins, and have devastating effects on public health. More than one billion people are estimated to be affected by NTDs, and further than one billion are vulnerable. NTDs are mainly endemic in countries having poor socioeconomic status [3].
NTDs disproportionately affect impoverished people; those who have limited access to clean water, sanitation, and primary health facilities that are indispensable to combat infections caused by certain pathogens.
Most are chronic, slowly progressing conditions that lead to severe health complications if left undiagnosed and uncured. They cause extreme discomfort, impair physical and mental health, deform the skin, and lead to many disabilities [4].
The individuals are subjected to social stigmatization, discrimination, and isolation due to their spoiled physical appearance. This kind of stigmatization causes them to suffer mentally, psychologically, and financially [5]. Therefore, NTDs coexist with poverty and further aggravate poverty.
Why they are termed “Neglected”?
The term “neglected tropical diseases” was minted by Dr. Peter Hotez and his colleagues in 2003 to counterpoise the focus given to HIV/AIDS, TB, and malaria [6]. They are called “neglected” because they are considered insignificant and are nearly absent from global health programs and policies. Combating NTDs still requires substantial funding and resources from global agencies [3].
Most Prevalent NTDs in Pakistan
Pakistan stands in the top 10 countries exhibiting the highest burden of NTDs for 8 out of 20 NTDs. Leishmaniasis, leprosy, trachoma, and soil-transmitted helminthiasis (STH) constitute the highest burden of NTDs in Pakistan [7]. Other NTDs that are also widespread include chikungunya, rabies, dengue, cystic echinococcosis (CE), venomous animal contact, typhoid, and paratyphoid fever [7,8].
In this article, we will briefly explore the most prevalent NTDs in Pakistan.
Leishmaniasis
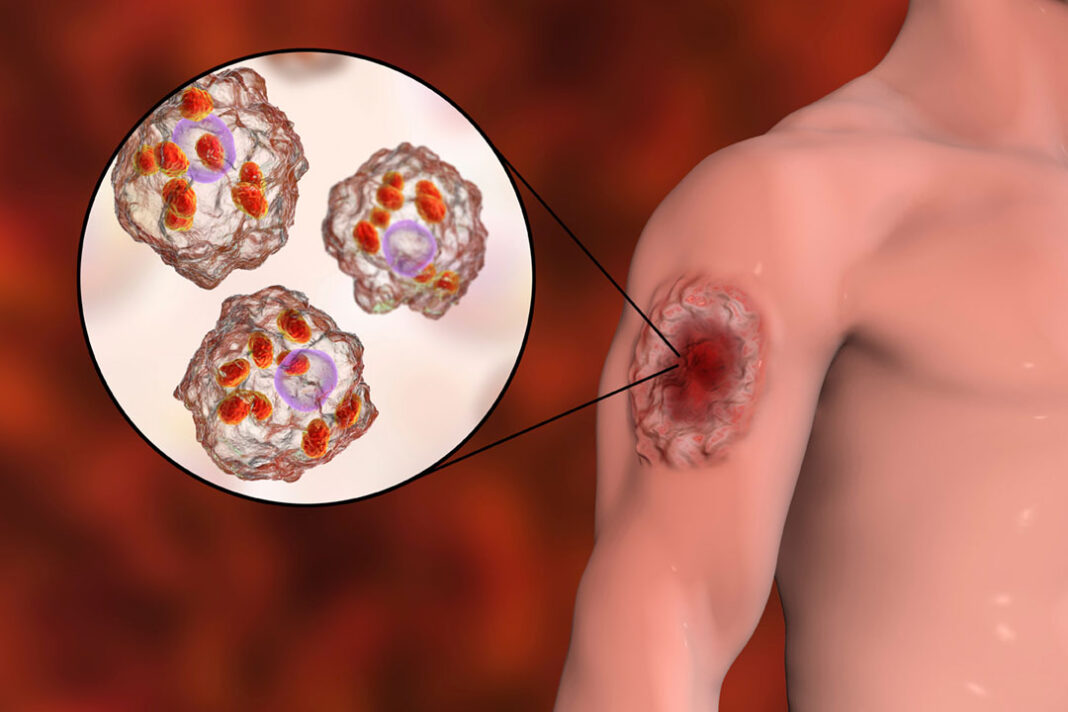
Leishmaniasis is an infectious disease caused by Leishmania parasites are transmitted by the bite of infected blood-sucking sand flies. However, people can get infections through the sharing of contaminated needles, and blood transfusions, and in some cases, a mother can transmit the infection to the offspring.
There are three major forms of leishmaniasis: visceral leishmaniasis (VL), cutaneous leishmaniasis (CL), and mucocutaneous leishmaniasis (ML). Only a smaller proportion of infected individuals ultimately develop the disease. Pakistan has a high burden of VL and CL.

“If you take leishmaniasis, a course of drug treatment would be equivalent to the loss of about six to nine months’ worth of income for an individual family in many parts of the world,” says Prof Paul Kaye, Hull York Medical School, UK (image credit: Dr. Tom Simpson)
- Visceral Leishmaniasis (VL): VL also called kala-azar, has 95 percent mortality rate if left uncured. It is characterized by intermittent episodes of fever, weight loss, splenomegaly (enlarged spleen) hepatomegaly (enlarged liver), and anemia.
- Cutaneous Leishmaniasis (CL): CL is the most common form and is characterized by painless skin sores that turn to ulcers and leave life-song scars on the body.
- Mucocutaneous Leishmaniasis (ML): It is characterized by sores in the mouth, nose, and throat and damage to the mucous membranes of these regions [9].
Leprosy
Leprosy is a chronic infectious disease caused by Mycobacterium leprae. The etiological agent of leprosy was discovered by Norwegian physician Dr. Gerhard Armauer Hansen in 1873, so the infection is also named “Hansen’s disease” [10].
The disease damages the nerves, skin, eyes, and Nose mucous membranes. It is characterized by disfigured and lumpy skin, painless ulcers, and torpor-affected body parts. In some conditions the patients get deprived of their senses of touch and pain, such cases are more prone to tissue injuries by cuts and burns. Besides fighting the infection, afflicted individuals have to endure social exclusion and intolerance [11].
One can get leprosy by inhaling the droplets released when the infected individual exhales, sneezes, or coughs. Prolonged close physical contact with uncured clinical cases culminates in catching the illness. It is unlikely to get infected through casual contact like shaking hands, hugging, or sharing things [12].

Trachoma
Trachoma is a bacterial eye infection that affects both eyes. Chlamydia trachomatis is the bacterium responsible for trachoma. At initial levels, it causes conjunctivitis (inflammation of the conjunctiva) or pink eye characterized by the dribbling of the eyes and itchiness of eyes and eyelids. As the condition advances, it results in pain and impaired vision.
If left uncured, culminates in scarring and causes the eyelids to move inward and this form of infection is called trachiasis. The eyelashes strike against the cornea, leading to corneal wounds and permanent visual impairment.
Trachoma is highly contagious and is transmitted via close physical contact with infected individuals, vectors (insects, flies), and contaminated inanimate objects [13].
The developed countries’ view of the diseases of the developing world is that only three are important: AIDS, tuberculosis, and malaria. But other infections, with names that most Westerners do not know – and often cannot even pronounce – kill, blind, deform, and disable far greater numbers of people. ~ David Molyneux, British parasitologist and former director of Liverpool School of Tropical Medicine.
Soil-transmitted helminth (STH) Infections
The word “helminths” has its roots in Greek meaning worms. STH infections are the most widespread parasitic infections that afflict the poorest with a limited supply of life-sustaining resources. The major species involved are roundworms, whipworms, and hookworms which cause ascariasis, trichuriasis, and ancylostomiasis respectively.
These worms reside in the intestine and produce eggs that are excreted out along with feces. Areas (soil or water resources) with inadequate sanitary facilities are contaminated by these eggs.
Ingestion of eggs via contaminated vegetables and water leads to the illness. Moreover, children can get infections while playing in the contaminated soil and then putting their hands in their mouths without cleaning them. Hookworms produce eggs in the soil, which release larvae that mature into infective forms. People catch the hookworm infection by walking unshod on the contaminated soil.
STH infections can lead to various symptoms including diarrhea, abdominal pain, loss of appetite, malnutrition, weakness, stunted growth, and development [14].
Control and Prevention
WHO proposed five strategies to intensify the prevention, control, elimination, and eradication of NTDs.
- Disease management: This strategy is aimed to address the diseases that demand individual-level care. Facilitating access to advanced diagnostic tools and prioritizing innovation in research and development of the tools and medicine are the core motives of this intervention.
- Preventive Chemotherapy: It emphasizes the need for proper administration of authenticated medicines to the eligible population.
- Vector Control: This approach signifies the scope of cost-effective and sustainable methodologies to prevent those NTDs whose spread is entirely dependent on vectors.
- Veterinary Public Health: This multidisciplinary approach highlights the coordination and collaboration between public health experts, veterinarians, and environmental scientists to combat and eradicate the NTDs that can be transmitted from animals to humans (zoonotic diseases).
- Water, Sanitation, and Hygiene (WASH): This strategy focuses on the dire need for the inclusion of a WASH component to mitigate the burden of NTDs as you know these diseases mostly afflict people with limited access to these basic resources [15]
The world has seen a significant change in the policies of global health authorities. What was considered neglected is now on the global health agenda as indicated by the 2021-2030 roadmap endorsed by the World Health Assembly to end NTDs.
Programs intended to eradicate NTDs should be unbiased and authorities need to ensure transparency in administrating drugs and providing funding. To reduce mortality, and morbidity and ease the sufferings of the poor, cooperation between the health systems of developing and developed countries is inevitable.
“The treatment and prevention of NTDs not only saves lives but also improves childhood development, school attendance and performance, pregnancy outcomes, and worker productivity in the world’s poorest countries,” says Dr. Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine.
References:
- https://msfsouthasia.org/a-journey-to-healing-muhammad-usmans-battle-with-cutaneous-leishmaniasis/
- Karlijn Hofstraat, Wim H. van Brakel, Social stigma towards neglected tropical diseases: a systematic review, International Health, Volume 8, Issue suppl_1, March 2016, Pages i53–i70, https://doi.org/10.1093/inthealth/ihv071
- https://www.who.int/health-topics/neglected-tropical-diseases
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3756642/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10478415/
- https://tidsskriftet.no/en/2018/01/global-helse/neglected-tropical-diseases-present-and-future
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8039485/
- Blum AJ, Majid MF, Hotez PJ (2018) Pakistan: A nation held back by NTDs. PLoS Negl Trop Dis 12(10): e0006751. Doi:10.1371/journal.pntd.0006751
- https://www.who.int/news-room/fact-sheets/detail/leishmaniasis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8805473/#b4-1124-9390_29_4_2021_623-632
- https://www.cdc.gov/leprosy/about/index.html
- https://www.who.int/news-room/fact-sheets/detail/leprosy
- https://www.aao.org/eye-health/diseases/what-is-trachoma
- https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections
- https://www.who.int/teams/control-of-neglected-tropical-diseases/interventions/strategies
More by this author: The World Needs to Boost Biotechnology and Biomanufacturing Initiatives