Conventionally, infectious diseases were thought to be an environmental or extrinsic factor that spread through pathogenic microbes like bacteria, viruses, fungi, and various parasites. For this reason, killing infectious pathogens or avoiding the point of contact was thought to be the primary goal in preventing the spread of infections, also known as communicable diseases.
However, with the advent of ‘the genetic theory of infectious diseases in the 1920s, scientists and the world community understood better that various other factors are also responsible for the spread, as well as the aggressiveness of infectious diseases and the most critical of them all is the role of genetics.
Genetics, particularly genetic evolution, has played a pivotal role in infectious disease spread and its morbidity and mortality rates. Therefore, to control infectious diseases, it is imperative to understand the role of genetics in both the pathogen and host in affecting infection pathogenicity, transmission and spread.
Why do some people fight infections better than others?
Host genetic predisposition and asymptomatic nature of infectious diseases
Infections do not always show the same symptoms in everyone. Recently observed during Corona pandemic, many cases went undiagnosed as individuals showed no apparent infection symptoms (the asymptomatic cases) while others suffered normal to aggressive symptoms (the symptomatic cases).
This difference arises from the individual ‘Genetic Makeup,” which differs across a population, making the host immune stronger to fight against infection and therefore show no symptoms, or have weak immunity that leads to a slower response against the infection and therefore exhibits the disease symptoms. This ‘Genetic Predisposition’ leading to a weak response is primarily the result of mutations, making such individuals more vulnerable to infection and its spread.
To better illustrate the idea, let’s look into an example of AIDs by HIV infection, the susceptibility of which increases in individuals having mutated CCR5 (Chemokine Receptor 5) gene. CCR5 is a crucial component of the host immune response signaling expressed on lymphocytes, a key player in the immune system. In addition, the HLA (Human Leukocyte Antigen), a gene complex, is a significant factor in host immune response and susceptibility to various infections.
Genetical evolution in infectious pathogens
Pathogens constantly strive to adapt to the environment, undergoing constant genetic evolution, making them more virulent, and aiding their survival.
“Not only the host, but genetic variations in pathogens also affect the disease outcome”
The main culprit behind infections getting severe, resistant, and transmissible is the genetic evolution of pathogens causing them. This genetic evolution in microbial genomes often results in new strains that may resist previous treatments. This happened when MRSA (Methicillin Resistant Staphylococcus Aureus) strain, causing most skin infections, emerged out of S. aureus (Staphylococcus aureus).
Genetic evolution may also result in novel disease emergence, as it happened in the case of coronaviruses acquiring repeated mutational and recombinational variations, resulting in a novel variant, SARS-COV-2, responsible for the Covid-19 pandemic.
How do infectious pathogens acquire genetic variability to evolve?
Different genetic processes make pathogens evolve and thrive in the environment. Some of these are: “Mutations, Recombination, Horizontal Gene Transfer, and Selection Pressure”.
Genetic mutations
Pathogens primarily depend on their power to rapidly mutate their genetic makeup, allowing them to survive in the environment. These mutations may be spontaneous (happen during DNA replication) or induced by the environment. Environmental factors are particularly important to understand as they may help us control pathogen evolution.
The environment-induced mutations mostly happen when drugs, chemicals, or radiations are employed with the intention of wiping out pathogens. However, it results in new and resistant strains. An exciting example is the influenza (flu) virus, which undergoes rapid mutations inside the host, changing its surface proteins to evade host immune recognition.
Genetic recombination
This method of achieving genetic variability is quite interesting. Genetic recombination involves the exchange of genetic material between 2 different strains of the same pathogen, particularly when they come close together while infecting the same host. This lets new pathogenic strains emerge, showing improved virulence and survival features. Genetic recombination of influenza viral strains between domestic livestock and humans may result in severe consequences such as a pandemic.
Horizontal gene transfer
This process usually occurs in bacteria and plays a critical role in bacterial evolution. Horizontal gene transfer is an inverse process of vertical gene transfer. Whereas vertical gene transfer allows the transfer of genetic material and traits from parents to offspring (same species), horizontal gene transfer lets two distant species (not related by descent) share genetic material.
Horizontal gene transfer may be accomplished through any of the following three methods:
Conjugation, where two cells directly exchange DNA by fusing at conjugative pili or through plasmids, e.g., Agrobacterium tumefaciens and E. Coli undergoes conjugation.
Transduction, where viruses called bacteriophage infect different bacteria, injecting the DNA from one to another e.g., E. coli bacteria has been transduced through lambda phage virus to allow it to use biotin and galactose.
Transformation, which allows the integration of foreign DNA, is taken up by a competent cell. These processes have resulted in various antibiotic, drug, and pesticide-resistant bacteria e.g., Streptococcus pneumonia.
Selection pressure
This allows infectious pathogens to thrive by adapting to their environment. Selection pressure is the external force that makes a pathogen evolve to suit its survival better. These pressures may include host immunity, transmission mode, host population pressure, or any danger in the environment, such as drugs, vaccines, and antibiotics used to stop pathogenic growth.
This has resulted in bacteria that have adapted to thrive in the presence of multiple antibiotics and viruses with more substantial virulence (the ability to cause disease). An interesting example of adaptation to population and immune pressure is the evolution of the influenza A virus into the H1N1 subtype, which caused a severe pandemic in 1918, leading to a high mortality rate.
Genetical evolution and the spread of infectious diseases
A solid and direct relationship exists between genetic evolution and the broader spread of infections. Infection transmission and spread greatly depend on the host’s genetic susceptibility and the microbe’s genetic and pathogenic factors.
Hosts with weaker immune are more susceptible to infection, allowing pathogens to survive and transfer to the other hosts e.g., CCR5 (Chemokine Receptor 5) mutated hosts are more susceptible to AIDs. Another relevant example is the mutated human DARC (Duffy Antigen Receptor of Chemokine) gene which allows malarial transmission.
On the other hand, genetic factors of the microbe make them more pathogenic and virulent. Let’s look into the example of the influenza virus that undergoes mutations to change its surface proteins and evade host immunity. This lets the virus survive, multiply in huge numbers, and quickly spread out to the other hosts. Another example is the genetic evolution of HCV (hepatitis C virus), which lets it transmit through multiple routes to infect a larger population.
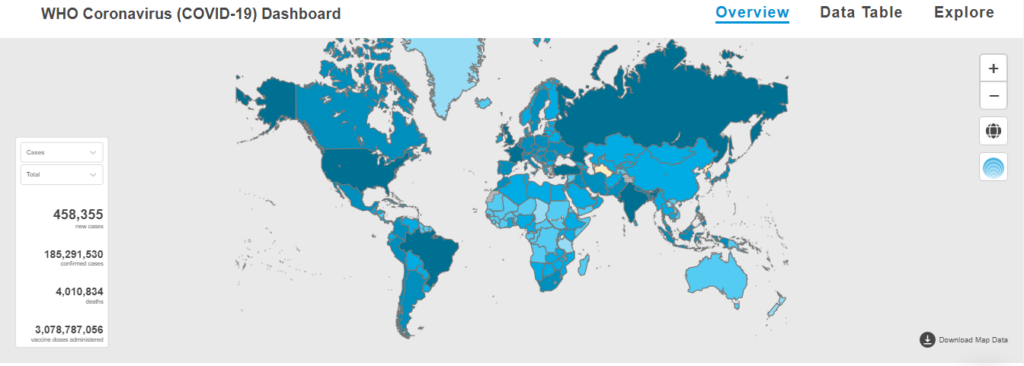
In the case of COVID-19, the genetic change in viral surface receptor ACE2 (Angiotensin Converting Enzyme 2), allowed it to transmit and enter the host cells efficiently. In addition, many pathogens spread among hosts by genetic changes in genes responsible for virulence and transmission, such as toxins and adhesins e.g., S. aureus (Staphylococcus aureus) spreads to the host by using its antibiotic resistance ability provided by the SCCmec (staphylococcal cassette chromosome mec).
What next? Genetic-associated preventive measures!
Our understanding of host and pathogen genetics has led to a safer and more effective design of preventive measures and infection treatments. We have all witnessed the consequences of drug misuse, such as antibiotics which have resulted in the emergence of more virulent and resistant bacterial strains.
Today, individuals can opt for personal genetic testing and screen out any possibility of infection susceptibility. This will help take early precautions and avoid catching an infection by undergoing timely vaccination or prophylactic treatment to stay on the safer side.
On the other hand, genetic sequencing of the pathogen genome helps track new mutations and identify any new strain emergence. However, genetic preventions come with a price of high ethical concerns. Genetic testing of individuals may put them in an uncomfortable spot where they may face discrimination or stigmatization. In addition, gene editing and genetic therapies raise concerns for equal accessibility by all, their long-term efficacy, and safety concerns for the world’s ecosystem.
Conclusion
Host and pathogen genetic variations play a crucial role in spreading infectious diseases. Understanding the genetic evolution and genetic factors involved in infectious diseases’ spread has helped design more effective and specific preventive solutions. Advancements in genetic technologies, such as gene editing and gene therapy, offer promising prospects for controlling and eradicating infectious diseases. However, these techniques are yet costly and thus not accessible to everyone. Our aim should be eradicating this difference in the future and making genetic treatments reachable to everyone.
Also, Read: Chronic diseases: An interplay of infections and our genome
Gull-e-lalah is a former intern at Scientia’s Science Writing Internship (cohort 1) and later, working as a team member. She is a scientist, working in the field of Biotechnology and Molecular Pathology, and has a strong passion for science writing, demonstration and teaching.